- Researchers think there may be a better coronavirus cure than remdesivir and dexamethasone for severe COVID-19 cases that can lead to complications and death.
- A study says that the use of interleukin-6 inhibitors like sarilumab and tocilizumab in patients who require supplemental oxygen and ICU care may significantly reduce mortality and speed up recovery times.
- The potentially life-saving therapy was first proposed earlier this year, as other researchers have been looking at reducing the inflammatory response in patients who develop COVID-19 complications.
- This study’s conclusions may be useful in future research but it wasn’t a randomized, double-blind placebo-controlled study, which is the medical standard for the approval of new therapies.
The first novel coronavirus vaccines may receive regulatory approval as soon as October or November, and some categories of patients could soon be immunized to reduce the risk of infection. But it will take a long time for the general public to get access to these drugs, and many years for the world’s population to be covered. That’s why vaccines alone can’t bring us closer to having things return to normal. Effective therapies that can prevent severe complications and death will be key for managing the health crisis in the coming months. Drugs like remdesivir and dexamethasone work, but they’re not quite the magical cures doctors are looking for. We may never find a drug that qualifies as an all-in-one solution to prevent deaths and improve recovery time. But some researchers think they’ve found a drug that may work better than remdesivir and dexamethasone on patients who end up on ventilators and who are at risk of dying.
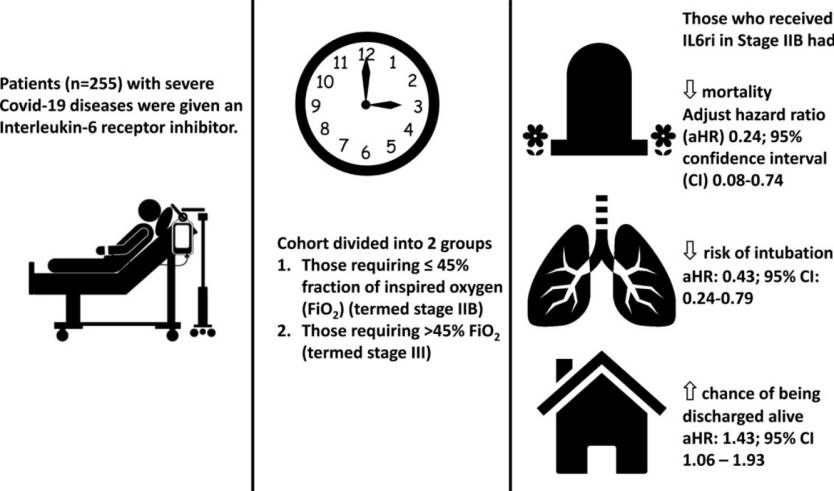
Doctors from Boston Medical Center (BMC) divided a group of 255 COVID-19 patients who needed oxygen therapy into two groups depending on severity, stage IIB (149 people) and stage III (106 patients). The doctors treated the patients with Interleukin-6 (IL6ri) inhibitors like sarilumab or tocilizumab. These are drugs that are already used with autoimmune diseases like rheumatoid arthritis as well as other inflammatory conditions.
These drugs can deal with the so-called cytokine storm that can occur in some COVID-19 patients, a condition where the immune response doesn’t just attack the pathogen and the infected cells but also healthy tissue.
Doctors first proposed therapies based on IL-6 inhibitors back in April to reduce the inflammation in the body and help the patients to breathe without a machine and eventually heal. We learned in mid-June that remdesivir maker Gilead Sciences is looking at improving COVID-19 therapies, with one idea being the combination of remdesivir and tocilizumab. A separate study that everyone should have handy, whether they’re doctors or patients, explained all the ways COVID-19 hurts the body, including the cytokine storm.
Getting back to the Boston University study that was published in the International Journal of Infectious Diseases, the doctors observed that administering IL-6 inhibitors earlier in the therapy of the 255 patients was more effective.
Initially, the doctors used the drug on stage III patients or people with higher supplementary oxygen requirements, but then the drugs were added to the stage IIB group as well. The BMC researchers observed that patients who received IL-6 inhibitors had a lower mortality rate than patients who were part of the intervention and control groups of remdesivir and dexamethasone studies.
The mortality rate for 105 patients who required ICU was 22.9%, considerably lower than the 45-50% mortality rate in other coronavirus studies. “In aggregate, IL6ri use was associated with decreased mortality, decreased rate of intubation, higher likelihood of being discharged alive, and shorter length of stay,” the researchers wrote.
“The greatest benefit of IL6ri use was seen in patients who received the drug in an earlier stage, prior to critical respiratory decompensation, showing the importance of prompt testing and treatment,” study researcher Pranay Sinha said. “We hope these findings can help guide physicians as we seek solutions to reduce mortality, increase extubation, reduce the length of stay in the hospital, and have more patients discharged from the hospital alive.”
That said, the study does have a significant “problem” that needs to be addressed in further research. This was observational research, meaning there was no control group given a placebo to measure the effectiveness of IL-6 inhibitors in COVID-19 management objectively. The comparisons to remdesivir and dexamethasone might not be objective either. Still, the study has been peer-reviewed and the BMC doctors aren’t the only ones looking at IL-6 inhibitors as a potential tool for preventing the life-threatening cytokine storms that occur in some at-risk patients. The full study is available at this link.








