- The list of coronavirus symptoms is long, although most of them can also appear in other medical conditions. That’s why a positive diagnosis requires a PCR test.
- The virus has been found to affect the eyes, with healthcare workers describing COVID-19 patients with red eyes or pink eye symptoms.
- A study details the case of a young woman whose main reason for going to the doctor was redness and discharge in her eye, a condition the doctors later diagnosed as keratoconjunctivitis.
- The patient displayed mild respiratory symptoms and did not qualify for a COVID-19 test initially. After several visits to ophthalmologists, she was finally tested, with samples from her eye also testing positive for the virus.
The clinical presentation of COVID-19 can include a variety of symptoms, but not all patients exhibit the same signs, and many infected people are asymptomatic. The novel coronavirus doesn’t even have that many specific signs that would allow physicians to diagnose the infectious disease without a PCR test. The sudden loss of smell and taste is one such unique symptom that’s likely to appear after a COVID-19 infection. But not for everyone.
That’s not the only downside of these unspecific COVID-19 symptoms. You might freak out whenever you experience a potential COVID-19 symptom, as you’ll have no way of knowing whether it’s the virus or something else. Only a test can bring you peace of mind, because the virus can infect various parts of the body, not just the lungs. The eye is one location where the virus can multiply, giving you a red eye or pink eye condition that you wouldn’t necessarily associate with COVID-19. However, you should absolutely be aware of this possibility, as this manifestation of COVID-19 could be serious, and could even impact your eyesight.
A nurse in Kirkland, Washington said back in late March that every patient she’d seen after testing positive for coronavirus had red eyes. They called the phenomenon “allergy eyes” because allergies can give you the same condition. Other healthcare workers noticed the same symptom in Canada in early March, detailing a case of keratoconjunctivitis in a 29-year-old patient who experienced no other major signs of COVID-19 infection. The study was published in The Canadian Journal of Ophthalmology.
The young woman spent a month in the Philippines and one day in San Francisco before returning to Canada. After one day of experiencing conjunctivitis, a clear watery discharge, and photophobia in her right eye, she went to an eye doctor. Other symptoms included rhinorrhea, cough, and nasal congestion, which we now know can be caused by COVID-19. She did not have a fever, but the medication she took over the counter may have masked it.
She returned on February 29th and went to the hospital multiple times in early March with worsening eye-related symptoms. She was diagnosed with keratoconjunctivitis, which is a complex eye condition.
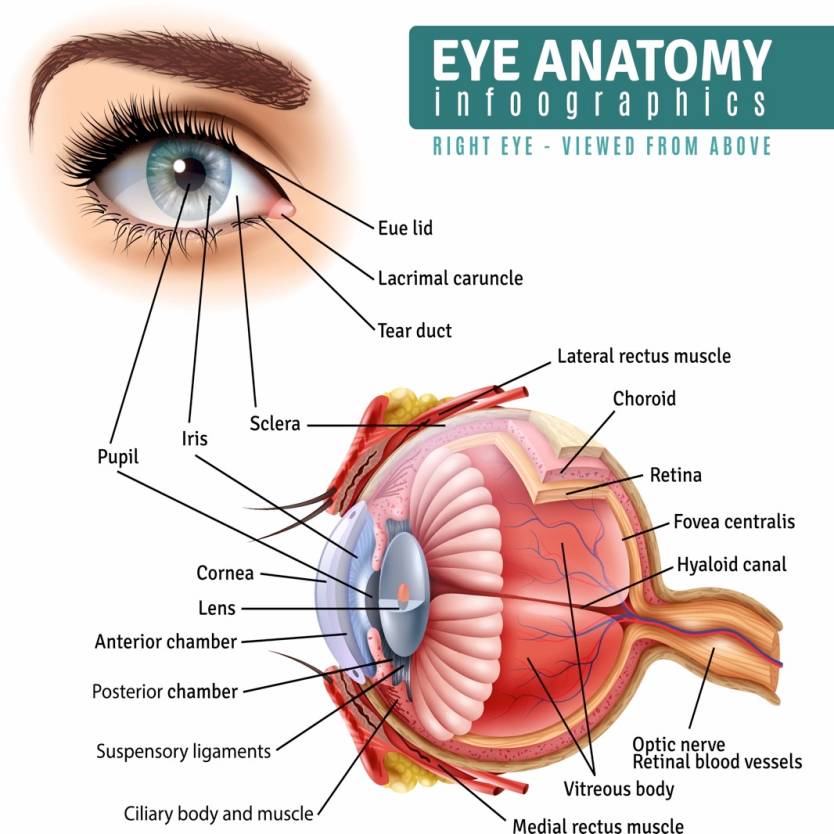
As the name suggests, the diagnosis is comprised of two distinct elements. Keratitis is the inflammation of the cornea or the transparent part of the eye in front of the pupil and the iris. Conjunctivitis, meanwhile, is the inflammation of the transparent tissue that covers the white of the eye and the surface of the eyelid. In either case, you might refer to it as a red eye or pink eye — the illustration above shows the anatomy of the eye.
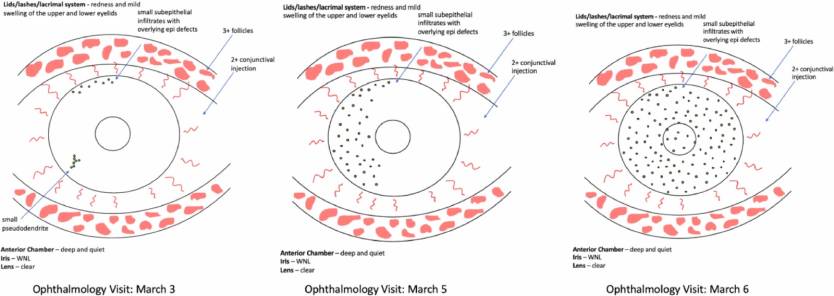
Now, here’s an image of the patient’s eye taken before her second visit dated March 5th:

Her eyesight was not impaired after the first two visits, but on March 5th, her vision had started to decline from 20/20 visual acuity to “20/40 pinhole to 20/30.” Further examinations revealed epithelial damage and the patient continued the prescribed treatment for her condition. She did not qualify for COVID-19 testing according to the Canadian protocols at the time, but doctors had collected eye swabs to test for chlamydia, gonorrhea, and bacterial culture. The tests were negative, but the tests were later used to check for the presence of SARS-CoV-2 in the eye.
By March 6th, COVID-19 testing in Canada had changed, and she qualified for testing. A PCR test on March 8th was positive, and then samples from her eye were tested as well, confirming that the virus was present for the lesions in the eyes.
“To the best of our knowledge, this is the first reported case of COVID-19 (caused by the SARS-CoV-2 virus) presenting with keratoconjunctivitis as the main symptom,” the researchers concluded.
“The patient did not present with conjunctivitis as previously reported for COVID-19 cases, but as keratoconjunctivitis. It was also apparent from the clinical examinations that the epithelial defects varied from one examination to the next and appeared as a pseudodendrite perhaps from a healing epithelial defect or possibly as a progressing subepithelial infiltrate.”
“The patient’s primary symptom and reason for repeatedly seeking care was a red eye with watery discharge,” the study reads. If you’re experiencing similar eye issues, you should consider the possibility of being infected with SARS-CoV-2. The CDC has a thorough list of coronavirus symptoms that you should check out if you suspect an infection. The New York Times created an interactive infographic that shows the most common symptoms associated with the illness.
The researches warn that healthcare workers treating patients that manifest such symptoms should know that a red eye could be an indication of COVID-19. “Patients who have a red eye; respiratory symptoms such as cough and shortness of breath; and recently traveled to areas with known outbreaks are at higher risk of having COVID-19,” the doctors note. “Clinical interactions with any patients presenting with similar upper respiratory tract symptoms should be done with mouth and eye protection routinely if exposure to the patient’s secretions is possible.” n this particular case, five physicians and three healthcare workers had to be placed in self-isolation for 14 days after treating the woman.








