- The novel coronavirus symptoms are so varied and unusual because the pathogen can affect various organs, not just the lungs, which is the primary target for SARS-CoV-2.
- A new study explains in great detail how the coronavirus attacks the entire body, listing the organ-specific manifestations as well as courses of action.
- The study provides ample information about the severity of COVID-19, which should satisfy the curiosity of anyone looking to better understand COVID-19, including past, current, and future patients. It can also offer guidance to inexperienced physicians who haven’t had to deal with significant outbreaks in their communities.
The world has been battling the novel coronavirus for more than seven months, and we’ve had plenty of time to learn that COVID-19 is nothing like the flu, even though some people still dismiss it as such. It’s highly infectious, and its mortality rate is higher than influenza. It can’t be treated as effectively as the flu, and the drugs we take to treat flu symptoms aren’t enough to treat COVID-19. The complications are also far worse than the flu, and many people who have survived the infections will need months to truly recover.
That’s because the virus doesn’t just hurt the lungs and potentially destroy them. SARS-CoV-2 can impact several other organs, including the brain, heart, kidneys, gastrointestinal organs, liver, and skin. This explains the garden variety of symptoms that can be associated with COVID-19, and why most of them aren’t specific to the disease. For example, we learned in the first months of the European and American outbreaks that some people can exhibit stroke and heart attack symptoms that are actually caused by COVID-19. A brand new study provides an exhaustive list of medical conditions secondary to COVID-19 that should make it clear to anyone that the illness is nothing like the flu, and that the virus can trigger additional health issues, including life-threatening complications.
Doctors from the Columbia University Irving Medical Center in New York City that have been dealing with the virus for months published a study in Nature a few days ago. The paper details all the extrapulmonary health issues that can arise after contracting COVID-19, complete with management suggestions.
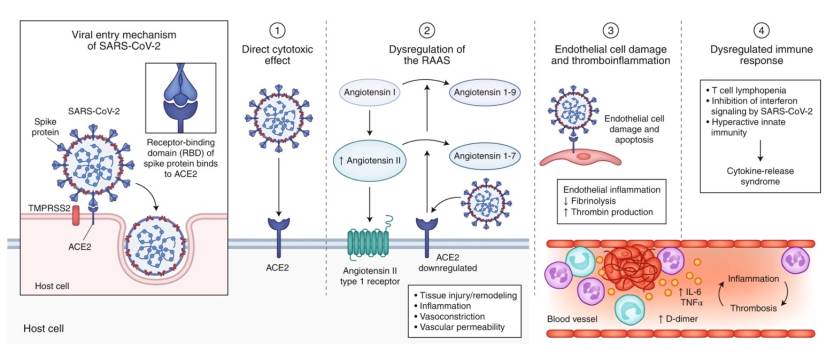
The work is incredibly detailed, and it’s the kind of scientific work that COVID-19 skeptics should inspect. Potential patients need to understand how dangerous the virus can be for the entire body, not just the lungs. The virus can bind to ACE2 receptors anywhere it finds them, not just the upper and lower respiratory tracts. The respiratory complications may be the most frequent, as shortness of breath can quickly escalate, and patients can end up on oxygen therapy and ventilation. Fewer people die now than in previous months after going on respiratory machines, but the death toll is still significant.
But the virus will bind to ACE2 proteins in other organs. It will clot the blood, inducing strokes and heart attacks, and potentially make it even more difficult to breathe. It’s not just that the lung tissue is destroyed as the virus replicates — so gas exchange isn’t possible — but if the blood clots in tiny vessels, then there won’t be any gas exchange in the areas of the lungs that aren’t affected by the virus.
The immune response also plays a massive part in recovery. It can neutralize the virus and kill the infected cells. But the immune response can go into overdrive and attack healthy tissue in the process. Other organs could be directly impacted when this happens.
The following infographic from the study briefly lists all the extrapulmonary effects of the virus. The study also includes a more detailed look at the manifestation of COVID-19 on each organ, complete with symptoms and management advice:
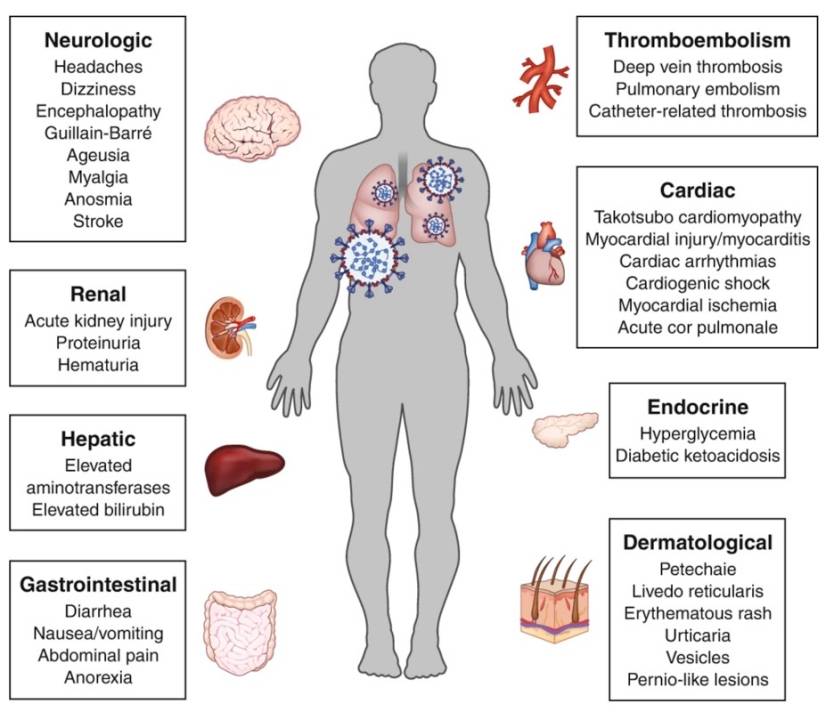
“Beyond the life-threatening pulmonary complications of SARS-CoV-2, the widespread organ-specific manifestations of COVID-19 are increasingly being appreciated,” the researchers wrote.
The Irving Medical Center’s research could also help physicians around the world who haven’t dealt with significant outbreaks so far and could help to guide other researchers who are studying the virus. The authors indicate several areas of research that could benefit for more work:
Some examples of areas that require further attention include elucidation of the mechanism by which SARS-CoV-2 is disseminated to extrapulmonary tissues, understanding of the viral properties that may enhance extrapulmonary spread, the contribution of immunopathology and effect of anti-inflammatory therapies, anticipation of the long-term effects of multi-organ injury, the identification of factors that account for the variability in presentation and severity of illness, and the biological and social mechanisms that underlie disparities in outcomes







