- New Infectious Disease Society of America guidelines say coronavirus antibody tests are pointless.
- Serological tests might not be able to confirm a prior COVID-19 infection if the illness occurred more than a few months ago.
- The society identified three scenarios where antibody tests can be useful, but even then, they’d have to be high-quality tests that correctly determine the presence or absence of antibodies. Most commercial tests might not meet IDSA’s recommendations.
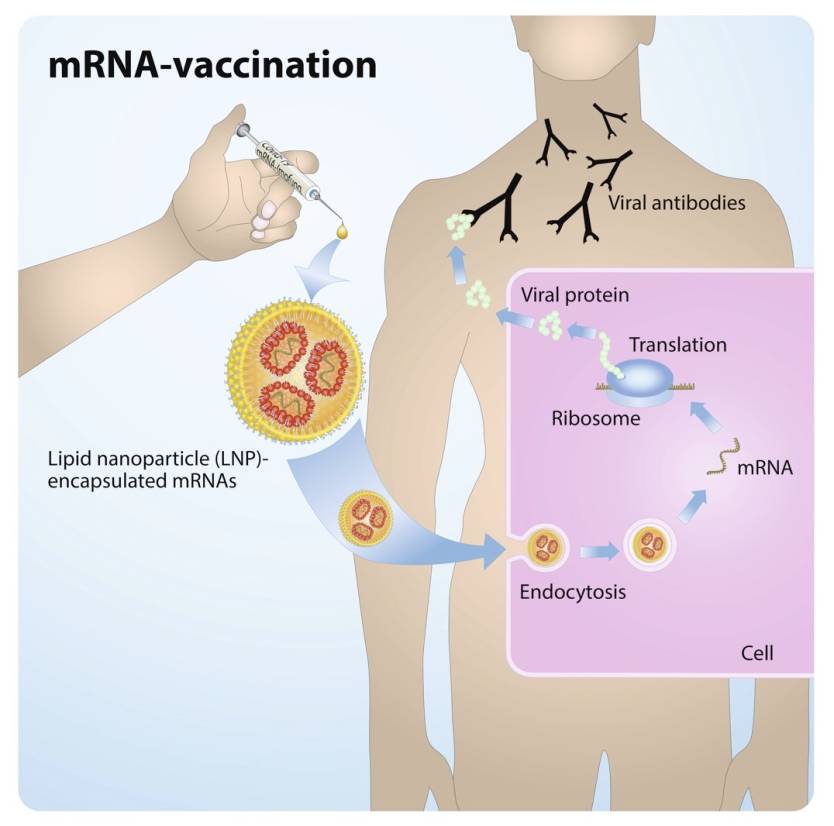
You’ve heard about them everywhere since the beginning of the health crisis; antibody tests that can tell you whether you’ve had an undiagnosed COVID-19 case in the past and whether you might be immune to the illness. Apply that concept to an entire community and you can determine the real rate of COVID-19 penetration. Studies from Spain and comments from the CDC said in the past few months that the actual infection figure might be close to 10 times higher than what has been reported. Antibody tests are also needed in vaccine trials, to prove whether the immune system has started raising armies of antibodies that might block the virus once the real thing comes along.
But recent studies have shown that antibodies wane in time, and they might disappear from the bloodstream entirely within three months. COVID-19 immunity isn’t lost when that happens, as hordes of T cells retain a memory of the infection and can help kill the pathogen upon reinfection. Studies also showed that current antibody tests could give false-negative results in patients who had COVID-19 in the past.
This all brings us to new guidelines that say antibody tests are pretty much pointless for individuals, although there are instances where they may be useful.
The Infectious Disease Society of America (IDSA) published an extensive paper on COVID-19 serologic testing.
The organization found that antibody testing isn’t good enough to “determine immunity or risk of reinfection.” The tests “cannot inform decisions to discontinue physical distancing or lessen the use of personal protective equipment.” That’s a more complex way of saying that you’re out of luck if you’re trying to determine whether that cold or flu-like illness back in February of March was really COVID-19. Another implication is that the so-called immunity passports that people keep talking about are completely out of the question. If current antibody testing isn’t good enough to prove someone had COVID-19, they can’t be used for issuing any sort of documentation that would say as much. And antibody testing is the only way hospitals can quickly check COVID-19 immunity right now. T cell and B cell testing is far more complicated and not as widely available.
The IDSA panel does think that antibody tests have a few limited uses, including one that somewhat contradicts the previous point. The society says that antibody tests can be used in epidemiological studies looking at herd immunity in communities. But if antibody tests can’t detect older infections, as we’ve just established, those herd immunity studies might not paint an accurate picture of a city or country’s COVID-19 immunity. Tests could pick up patients who were recently infected but might miss others, which is precisely what a recent study showed. Therefore, such research would always deliver a lower percentage of immunity in a community.
IDSA says there are two clinical scenarios where antibody testing has potential utility. One involves the “evaluation of individual patients with a high clinical suspicion for COVID-19” who keep testing negative, or who do not have access to PCR tests. But even this sort of use might not always yield accurate results. The paper notes there may be issues with antibody tests that could hinder that work:
In general, IgM tests tend to have lower sensitivity to detect past infection than IgG or total antibody tests. Assays designed to detect and differentiate IgM and IgG in combination, where the detection of either IgM or IgG is used to define a positive test result, and IgA tests tend to have lower specificity to detect past infection compared to IgG only or total antibody tests.
IgM, IgG, and IgA are types of Y-shaped immunoglobulins, or antibodies. IgM antibodies appear later in COVID-19 than with other viruses, IgG antibodies are detectable two weeks after infection, and IgA antibodies aren’t as good as telling SARS-CoV-2 apart from other human coronaviruses.
The paper also notes that the sensitivity and specificity of IgG and total antibody counts are optimal three to four weeks after the onset of symptoms. By the time antibody tests are optimal, people who are suspected of having been infected might have already cleared the virus.
There is a third instance where serological testing might be useful, and that’s the “for assessments of suspected multisystem inflammatory syndrome in children.” That’s the MIS-C syndrome that some kids experience, which could be fatal.
Not all hope is lost for using antibody tests for mapping out COVID-19 immunity. But tests should have a high clinical sensitivity and specificity (over 99.5%) “to be of value.” Antibody test makers should come up with improved test kits that would have very low false-negative and false-positive results. Right now, it’s believed that many antibody tests are not accurate. Even for herd immunity studies, the ISDA panel advises that tests should be correctly positive 96% of the time, and correctly negative at least 99.5% of the time. The majority of test kits that the panel studied do not meet these standards, Dr. Angela Caliendo told The New York Times. Also, none of them are available for at-home testing. The best types of antibody tests are Elisa or CIA (chemiluminescence immunoassay), so that’s the kind of serological testing you should be looking for.
One of the problems with antibody tests in America is the Food and Drug Administration’s decision to approve them without reviewing safety and efficacy data. That decision was reversed in May, with the FDA giving test-makers 10 days to prove their assays were accurate. But on Wednesday, the Department of Health and Human Services said that labs that made their tests did not have to go through an FDA review anymore, per an executive order from Trump. The order does not apply to commercial tests, but the tests you can buy right now are still not good enough.
The IDSA’s antibody testing guidelines are available at this link.








