New Studies Reveal Very Good News About Coronavirus Immunity
- Scientists are getting closer to explaining coronavirus immunity after infection or after immunization with a potential vaccine.
- A new series of studies shows that the immune system is capable of mounting a strong response to the pathogen, even in asymptomatic or mild cases.
- The researchers can't conclusively determine how long COVID-19 immunity lasts, but they can prove that even people who do not show detectable levels of antibodies after the primary infection will be protected in the months that follow.
The novel coronavirus is just too new for scientists to figure out how long immunity might last. That's a key detail that will help with immunization protocols once vaccines are available, as well as public health campaigns for containing outbreaks and reducing infection rates. The longer the immunity lasts, the easier and faster the world will reach herd immunity through a combination of vaccinations and direct infections. And once a large enough number of people are immune to COVID-19, the transmission rate will drop significantly. The virus will continue to roam the planet just like the influenza viruses, and it will spark new outbreaks as well. But the pandemic can still be conquered and future COVID-19 outbreaks won't be as bleak.
New studies have given us the good news about immunity that we need right now, showing that the immune system has what it takes to combat reinfection even after antibodies disappear from one's system. These studies also show the immune system mounts a strong defense in asymptomatic and mild cases, though they can't supply the one immunity answer we all want most.
Researchers have been able to prove that infection with the virus will lead to temporary immunity in monkeys. Vaccine research has shown that various experimental drugs can elicit immune responses that are on par or better than the immune system's response to actual infection. But as scientists studied the virus, some bad news about immunity crept in. Some experts believe the COVID-19 protection could last between six to 12 months, as is the case with resistance to human coronaviruses that cause the common cold. Others discovered that neutralizing antibodies in the bloodstream disappear within three months.
Then the good news kept coming in. Immune protection doesn't disappear once antibodies are gone. T cells retain the memory of the novel coronavirus and can produce a new wave of neutralizing antibodies upon reinfection. Then we heard that T cells trained during common colds to recognize other human coronaviruses would kickstart a defense against the novel strain as well.
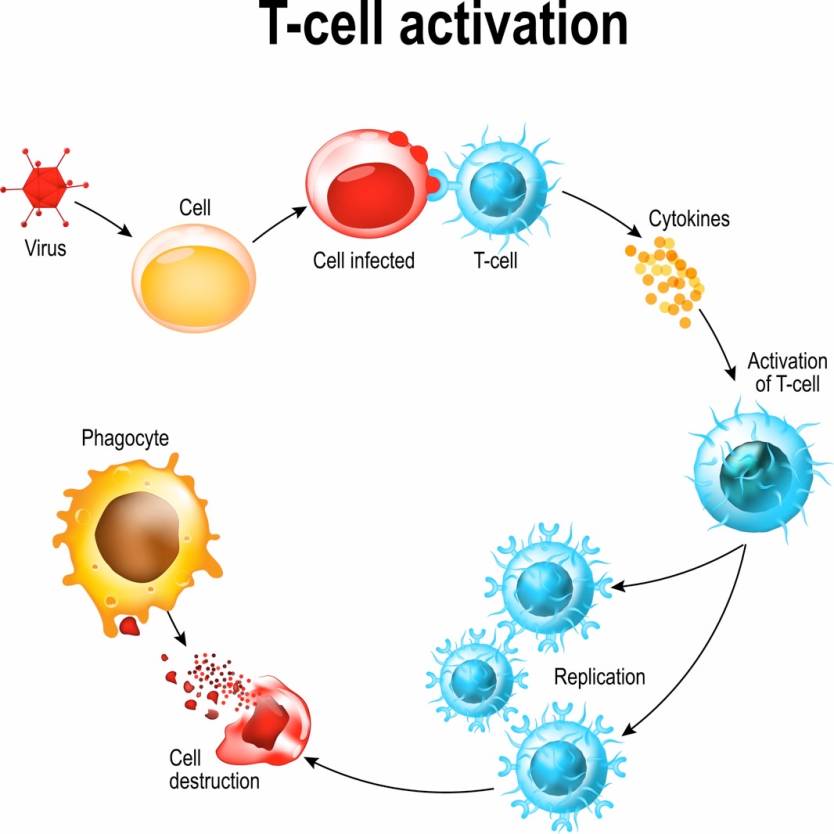
Diagram showing the activation of T cell leukocytes upon encounter with a pathogen.
A few days ago, the CDC quietly updated its COVID-19 quarantine guidelines with new information that says coronavirus immunity likely lasts for at least three months for people who were infected. This is the first time a health authority quantified COVID-19 immunity in some way. It may look like it's bad news, but as we explained, the CDC's findings aren't final. This is merely an indication that the CDC is confident enough that reinfection isn't possible within three months after the initial infection. Some people have tested positive again weeks after recovery, but all the data that we have so far indicates that's not reinfection. Traces of the virus may still be present in the body in a significant enough quantity to return a positive PCR test, but those patients are not infectious.
This brings us to a new set of research papers that indicate the human body has what it takes to deliver lasting immunity even after a mild case of COVID-19. The New York Times has highlighted a few new studies that address COVID-19 immunity, including research papers that haven't yet been peer-reviewed.
"Things are really working as they're supposed to," University of Arizona immunologist Deepta Bhattacharya told The Times. The researcher found that "the antibodies decline, but they settle in what looks like a stable nadir," which is about three months after the start of symptoms. "The response looks perfectly durable."
This is an indication that even if most antibodies have disappeared from the bloodstream, some of them still linger on. The B cells that produce them can either patrol the body or retreat inside bone marrow. It's up to the T cells to recognize the pathogen upon reinfection and activate the antibody-making B cells that will resume the fight.
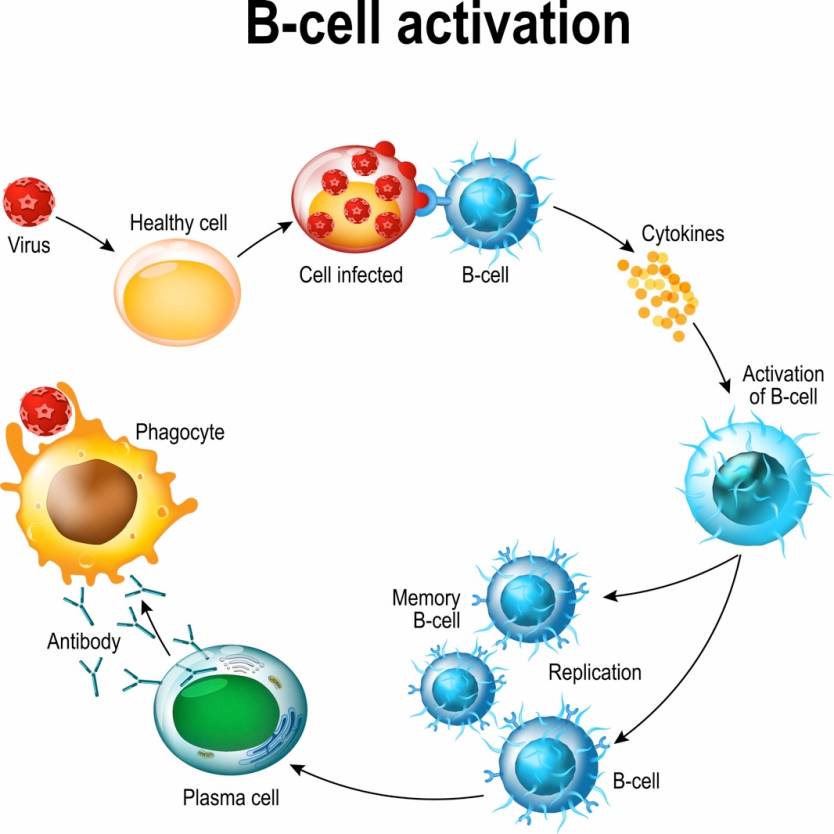
Diagram showing the activation of B cell leukocytes upon encounter with a pathogen.
"This is exactly what you would hope for," University of Washington immunologist Marion Pepper said. "All the pieces are there to have a totally protective immune response." Like Bhattacharya, Pepper's team found that antibodies linger on at low levels, which is evidence that B cells are still on watch. Pepper and her team collected B cell samples from patients who recovered from mild COVID-19 cases and grew them in the lab.
A different paper published in Cell showed proof that the body mounts a robust T cell response in COVID-19 survivors who were asymptomatic or had a mild case. The scientists took T cell samples long after symptoms disappeared and exposed them to the new coronavirus in the lab. The T cells were still able to deliver the right signals and cloned themselves to mount a defense against the virus.
Researchers from Canada looked for coronavirus antibodies in saliva and found that the Y-shaped proteins could survive for more than three months at the site of infection, or mouth, or nose. The researchers correlated the number of saliva antibodies with serum antibodies and concluded that the former can provide COVID-19 immunity.
None of these studies can tell us how long the immune response lasts, but they do prove that even people who don't experience a bad COVID-19 case will still have a lasting immune response. That's promising news for vaccines and herd immunity given that most COVID-19 patients out there develop mild COVID-19 infections, and many are asymptomatic. Previous studies have shown that antibody screening may deliver false-negative results for asymptomatic patients or people who only had moderate cases. The new research papers indicate that the presence of detectable antibodies does not tell the full COVID-19 immunity story.
Some of these studies have not been reviewed and more research is required on the matter of COVID-19 immunity, but this is good news. Proving that the body mounts a strong immune response to COVID-19 regardless of symptoms is only the first step. Researchers will also have to demonstrate that the immune response actually works upon reinfection — or that vaccines can indeed block the infection.
