4 Promising Coronavirus Cures Are Now Part Of A Massive Drug Megatrial
- The World Health Organization is spearheading a massive COVID-19 drug trial that will include thousands of patients in participating countries.
- The Solidarity megatrial will focus on four distinct therapies that include drugs that are already approved for other ailments, but have shown promise in treating some COVID-19 cases.
- The purpose of the study is to obtain more evidence about the efficacy and safety of these therapies, and hopefully device a standardized treatment protocol for those infected with the novel coronavirus.
- Visit BGR's homepage for more stories.
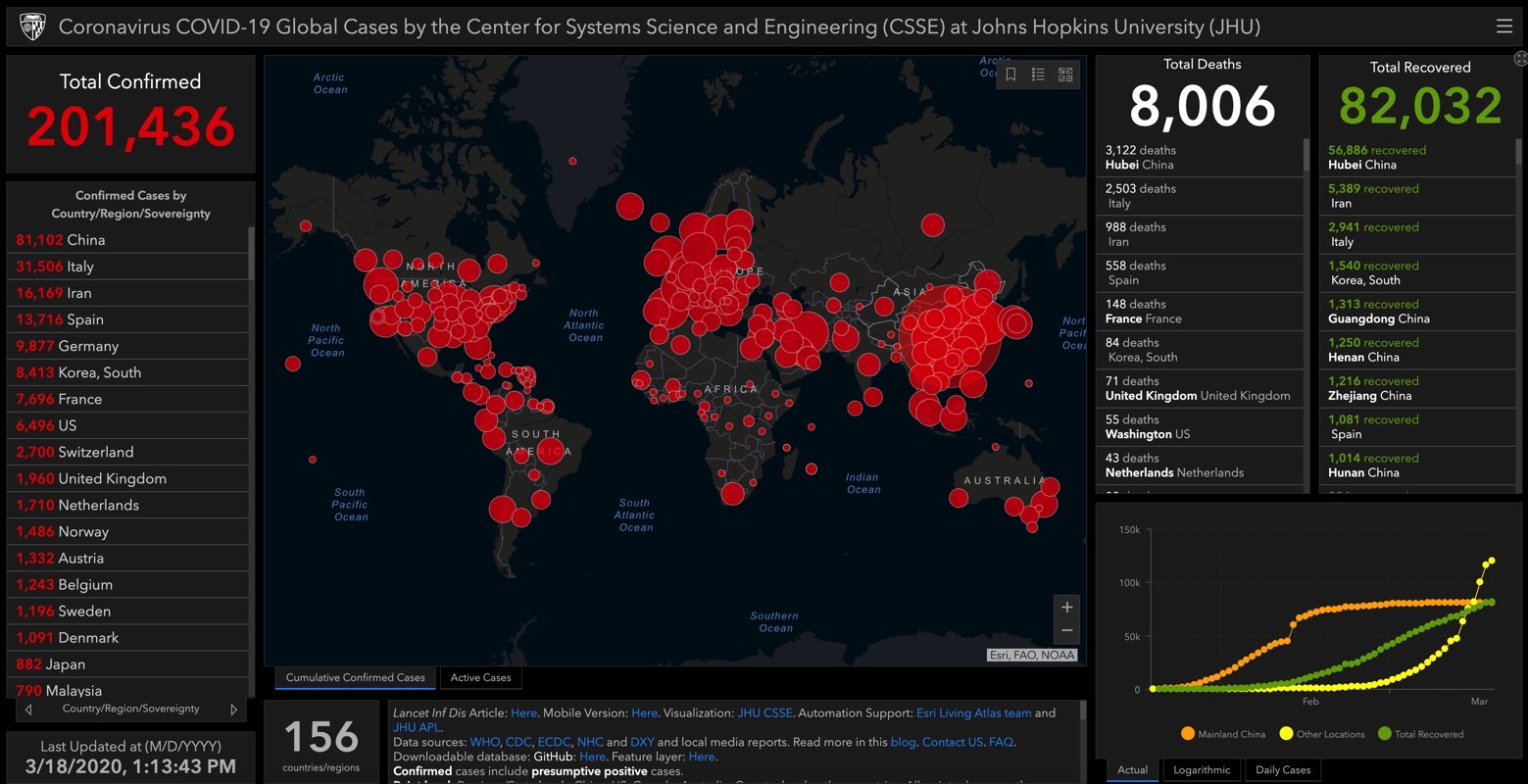
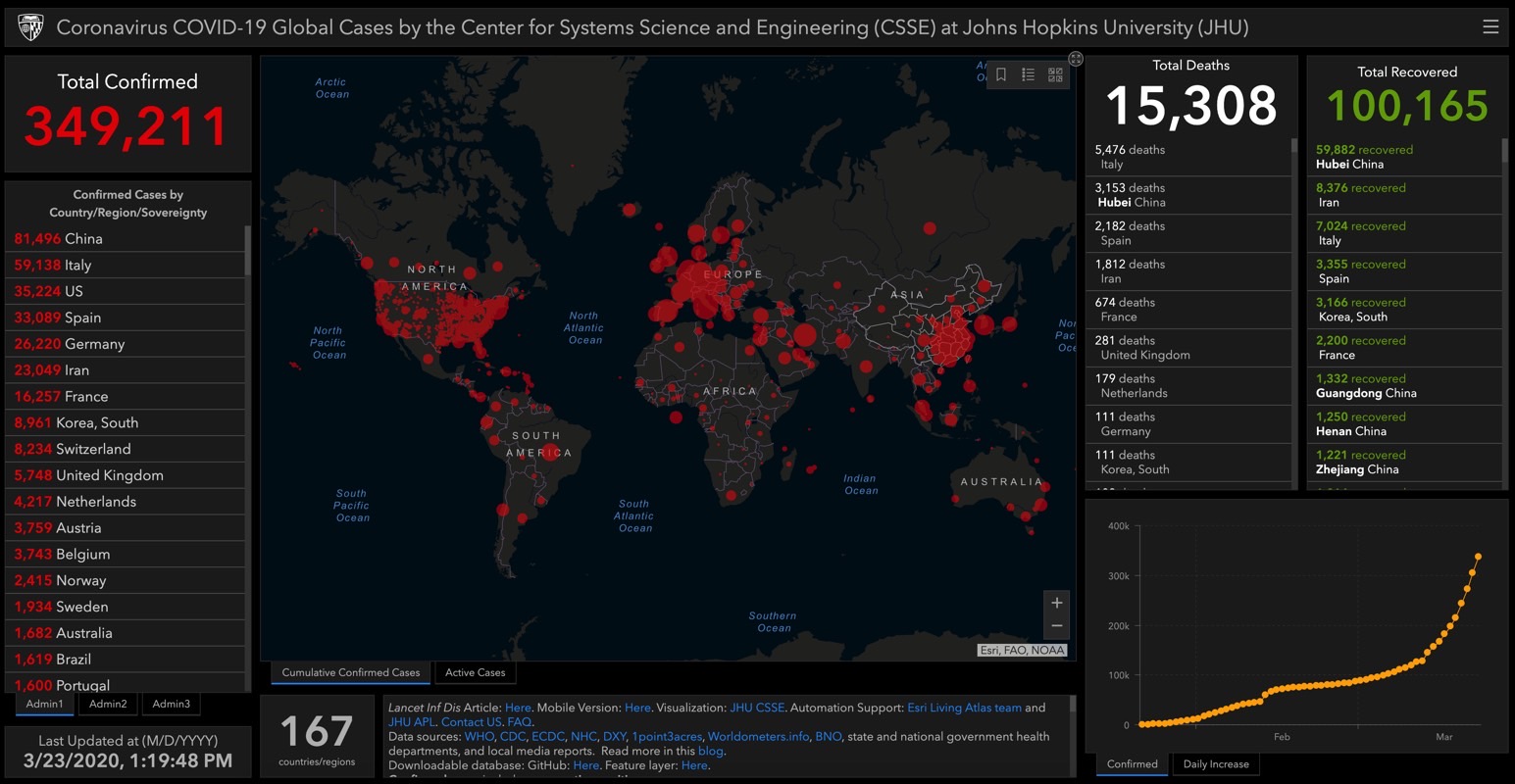
The World Health Organization (WHO) is working with its partners on at least 20 potential COVID-19 vaccines, which is the only type of treatment for the novel coronavirus that can eradicate the virus. That type of treatment is anywhere between 12 months to 18 months away, even though at least two clinical trials are already underway. In the meantime, the WHO is also conducting a separate effort to improve COVID-19 treatments, and the organization announced a massive megatrial that will focus on four different types of cures that have shown promising results in limited testing.
The object of this widespread testing is to allow physicians to offer patients the best possible care with the resources that are already available to them. Drugs that have been previously approved for use in treating other diseases could be used to improve the condition of the hundreds of thousands of patients who have been admitted to hospitals around the world, increase the recovery speed, and reduce the number of fatalities. Comparatively, developing a brand new drug specifically for the COVID-19 illness might take years, which is why WHO and participating countries are fast-tracking this worldwide trial of drugs that are already widely available.
The study is called "Solidarity" and it was announced a few days ago. It's meant to determine which of the four most popular therapies being used to treat COVID-19 are the most effective and safest for patients.
The Solidarity trial will include thousands of patients in several countries including Argentina, Bahrain, Canada, France, Iran, Norway, South Africa, Spain, Switzerland, and Thailand. ScienceMag also reports that the French National Research Institute for Medical Research (INSERM) is coordinating an add-on trial in Europe called Discovery that will include 3,200 patients from seven countries (Benelux countries, Germany, France, Spain, and the UK).
Solidarity and Discovery will be similar when it comes to the drugs that are being tested, except for chloroquine, which will not be included in the European-only trial.
Unlike regular clinical trials that are double-blind so that patients won't know if they're getting the drug that's tested or a placebo, the new studies will test the new therapies on all patients. Participating hospitals can enroll subjects with ease. The doctor will enter the patient's data in a WHO site, including preexisting conditions that could alter the course of the COVID-19 disease, and the participant will have to sign an informed consent form. The physician will also list the available drugs in the hospital, and the WHO will randomly assign the patient to one of the therapies available. After that, physicians will only have to record the day the patient leaves the hospital or dies, and whether he or she required oxygen or ventilation.
Remdesivir, a drug developed to combat the Ebola epidemic, appears to be the most promising of the four therapies, as the experimental drug has already proved to be effective against the SARS and MERS viruses.
Chloroquine and hydroxychloroquine may sound familiar, and that's because President Trump touted them on the news, saying they're "game-changers" and that he felt "good" about them. The significant attention the two drugs received recently may be the main reason the WHO is including these two drugs in Solidarity. Researchers in France also said the drugs showed promise treating COVID-19 but more extensive testing was needed. Some scientists worry that the doses needed to fight the novel coronavirus might be too high to warrant consideration. "Researchers have tried this drug on virus after virus, and it never works out in humans. The dose needed is just too high," University of Giessen pulmonary infections expert Dr. Susanne Herold told Science Mag. New reports reveal that the first cases of chloroquine poisoning appeared in Nigeria immediately following Trump's remarks.
Solidarity will also test a ritonavir/lopinavir anti-viral compound sold as Kaletra, which is included in HIV treatment. The combo was used in China with little success, but the study only included very-ill subjects, with more than a fifth of the 199 patients included in the double-blind test having died. The drug may have been given too late to make a difference.
Finally, the fourth therapy that will be tested by countries taking part in Solidarity and Discovery will mix ritonavir/lopinavir with interferon beta. This combo was used for MERS patients in Saudi-Arabia. The treatment may have unwanted side-effects if given too late though, and according to Herold, it could lead to "worse tissue damage instead of helping patients."
